ARTICLE SUMMARY:
Some 2.6 million Americans suffer a concussion/traumatic brain injury (TBI) each year, but there is as yet no rapid screening test that can accurately diagnose these patients at the point of injury. If such a test were available, concussion patients could take immediate precautions to avoid further brain injury and potential severe, lifelong effects. Several young companies are hoping to fill that unmet need with innovative new screening and diagnostic technologies.
With football season now in full swing, the topic of sports-related concussion and traumatic brain injury (TBI) is once again in the spotlight.
But concussion and TBI are not confined to the sports arena. Although sports-related concussions often make the headlines, people of all ages and occupations can suffer a concussion, whether as the result of a fall, a blow to the head, a motor vehicle accident, a battlefield explosion, or some other type of trauma. Researchers are just beginning to understand the seriousness of these events, particularly for those who have experienced multiple injuries, and they now realize that even mild concussions suffered in childhood can impact brain health decades later.
With a clearer view of the potential for severe consequences from repeated brain injuries, a number of young companies are racing to develop rapid, highly accurate and objective tests that can diagnose concussion and TBI immediately after the damage occurs so that steps can be taken to prevent further injury while the brain heals. Such tests would also help determine when it is safe for an athlete or soldier with a concussion to return to the game or the battlefield. Others are working on a variety of prevention strategies as well as new, more effective treatments for brain injuries and their aftermath.
Importantly, the implications of this work could go well beyond concussion and TBI. In fact, many of the diagnostic technologies currently being developed for TBI could find applications across a wide range of neurological disorders (and perhaps beyond); researchers are already considering their potential use for stroke, Parkinson’s disease, Alzheimer’s disease, and other disorders of the brain and central nervous system.
Historically, venture capital investment has been hard to come by for small companies working on novel TBI diagnosis and prevention strategies; however, the situation appears to be improving, with growing awareness of the scope and seriousness of TBI. Meanwhile, a number of other interested US stakeholders, including the sports industry, the US Department of Defense (DOD), and some large corporates in the medtech arena, have stepped in to help support promising early-stage research and development in this area.
One of the most ambitious projects currently underway in the private sector is the Head Health Challenge, an open technology competition sponsored in large part by medical imaging giant GE Healthcare and the National Football League (NFL). The aim is to uncover and help fund the development of promising new technologies with the potential to improve the screening/diagnosis, monitoring, and prevention of concussion and TBI. Although the NFL is a major supporter of the project, the technologies it is helping to fund could have an impact that goes far beyond the football field.
The competition is divided into three phases—the first, Head Health Challenge I—is focused on new technologies for diagnosing and monitoring brain injury, while Head Health Challenges II and III are focused on various ways of preventing brain injury using innovative biomaterials and real-time impact tracking technology. The final six winners of Head Health Challenge I (who were chosen out of more than 450 total entrants) were announced in late July and include three US universities, along with three young, innovative US-based device companies: BrainScope Company Inc., Quanterix Corp., and Banyan Biomarkers Inc., all profiled below.
Outside the scope of the Head Health Challenge, there are other large device companies working to improve concussion screening and diagnosis. In late September, Philips North America announced a collaboration with the Massachusetts Institute of Technology (MIT) to combine Philips’ ultrasound imaging technology with a physiological modeling algorithm developed by MIT’s Integrative Neuromonitoring and Critical Care Informatics Group. The goal is to develop a less-invasive way to measure intracranial pressure. According to Philips, intracranial pressure (ICP) is “an essential tool” for managing patients with brain injuries, but measuring ICP currently requires invasive penetration of the skull or lumbar spine. A less-invasive means to measure ICP could enable first responders to easily assess and monitor people with suspected concussion at the point of injury, in the ambulance, and in the emergency room.
Another large medtech company investing in this area is Abbott Laboratories, which has partnered with the US Department of Defense and Banyan Biomarkers to develop a blood test for concussion that will run on Abbott’s I-STAT point-of-care (POC) testing platform. In addition, computer giant Dell is working with the University of Mississippi Medical Center (UMMC) on a concussion telemedicine system for screening high school athletes. The pilot project, launched in August, is providing a cross-section of Mississippi high schools with a HIPAA-compliant platform consisting of Dell VSee software installed on Windows tablets equipped with high-definition cameras (Dell is furnishing both the software and the tablets). The system enables UMMC clinicians to virtually screen high school athletes with suspected concussion via video teleconference at the point of injury.
 The corporates have a deep pool of potential partners in the many young companies working in the field of concussion diagnosis and screening. Along with the Head Health Challenge winners and semi-finalists, listed in Figure 1, additional competitors (to name a few) include Cerora, which is developing a small (lighter-sized) EEG sensor and analytics system called CeroraBorealis that measures electrical activity in the brain and includes other parameters, such as voice analysis, to screen athletes for potential concussion; AnthroTronix Inc., an engineering R&D firm with a mobile brain health assessment app (DANA) that is FDA-cleared and works on smart phones and tablets—AnthroTronix won the Gold Edison Award earlier this year; and Jan Medical, developer of the Nautilus BrainPulse, a portable device placed on the head that analyzes brain pulse patterns.
The corporates have a deep pool of potential partners in the many young companies working in the field of concussion diagnosis and screening. Along with the Head Health Challenge winners and semi-finalists, listed in Figure 1, additional competitors (to name a few) include Cerora, which is developing a small (lighter-sized) EEG sensor and analytics system called CeroraBorealis that measures electrical activity in the brain and includes other parameters, such as voice analysis, to screen athletes for potential concussion; AnthroTronix Inc., an engineering R&D firm with a mobile brain health assessment app (DANA) that is FDA-cleared and works on smart phones and tablets—AnthroTronix won the Gold Edison Award earlier this year; and Jan Medical, developer of the Nautilus BrainPulse, a portable device placed on the head that analyzes brain pulse patterns.
 In order to be useful, diagnostics must link to helpful interventions. In the case of an isolated concussion, the best intervention is rest, which gives the brain time to fully heal. However, there is a great unmet need for more effective therapies to treat patients with more severe and lingering forms of TBI. Many pharmaceutical and device companies are investigating new ways of treating chronic TBI and its various clinical manifestations, with technologies ranging from stem cell therapies to neuromodulation devices.
In order to be useful, diagnostics must link to helpful interventions. In the case of an isolated concussion, the best intervention is rest, which gives the brain time to fully heal. However, there is a great unmet need for more effective therapies to treat patients with more severe and lingering forms of TBI. Many pharmaceutical and device companies are investigating new ways of treating chronic TBI and its various clinical manifestations, with technologies ranging from stem cell therapies to neuromodulation devices.
One company working in the neurostim arena is Helius Medical Technologies, which in August began enrollment in a 120-patient Phase III clinical trial in the US and Canada investigating its noninvasive Portable Neuromodulation Stimulator (PoNS) in patients with TBI-related chronic balance disorder. Developed in collaboration with the US Army Medical Research and Materiel Command, PoNS stimulates the cranial nerves in the tongue and is used in combination with functional therapy—such as physical, occupational, relaxation, and cognitive exercises—targeted to the patient’s specific deficits. (See “ Helius Medical Technologies: Using Neurostimulation to Help Retrain the Brain ,” this issue.) Helius is investigating the technology for multiple sclerosis as well, and says it could also have applications in stroke recovery, ALS, dementia/Alzheimer’s disease, and depression, a list that illustrates just how much potential clinical overlap there is in the neurological diagnosis/treatment arena.
TBI POC Diagnosis: A Massive Unmet Need
Traumatic brain injuries vary in severity, but mild injuries, or concussions, account for the majority (about 75%; note that the terms concussion and mild TBI are interchangea ble). Although a single, mild concussion typically will resolve without persistent negative effects, those who suffer multiple concussions—particularly when they occur in fairly rapid succession before the brain has time to fully heal—are at much higher risk of experiencing more serious and lasting symptoms. According to the Brain Injury Association of America, more than 5.3 million Americans are living with lifelong disability as a result of TBI. Some people with a history of repetitive brain trauma develop chronic traumatic encephalopathy (CTE), a progressive disease caused by a buildup of tau protein in the brain that is associated with devastating long-term consequences. That protein buildup slowly kills normal brain cells, resulting in a variety of severe symptoms that can include permanent cognitive impairment, memory loss, seizures, personality changes, and depression.
Along with the potential long-term impact of repeated brain injuries, there are also substantial costs in the short-term. In 2010 alone, TBI was a contributing factor in 2.2 million emergency room visits, 280,000 hospitalizations, 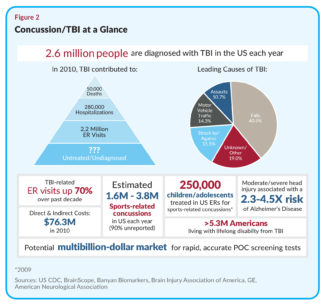 and 50,000 deaths in the US, according to the US Centers for Disease Control and Prevention (CDC), which says TBI contributes to about 30% of all injury-related US deaths each year. The direct and indirect costs of TBI to the US healthcare system was estimated at $76.3 million in 2010 (see Figure 2).
and 50,000 deaths in the US, according to the US Centers for Disease Control and Prevention (CDC), which says TBI contributes to about 30% of all injury-related US deaths each year. The direct and indirect costs of TBI to the US healthcare system was estimated at $76.3 million in 2010 (see Figure 2).
Although concussion and TBI can affect anyone, over the past few years, sports-related concussions have dominated the headlines, due in large part to events impacting NFL players and former players. But sports-related concussions in children are also raising alarms. According to the CDC, in 2009, US ERs treated nearly 250,000 sports- and recreation-related TBIs in children and adolescents, and that number has been rising steadily over the past decade. Many more likely go undiagnosed and untreated. The likelihood of suffering a concussion while playing a contact sport is as high as 19% per season of play, according to the University of Pittsburgh Brain Trauma Research Center.
Under Fire, the NFL Joins with GE to Tackle the Challenge
The NFL is one of the most active supporters of research in the sports-related concussion arena, and for good reason. In April of this year, the league settled a lawsuit brought by thousands of ex-NFL players who accused the NFL of trying to conceal the chronic impact of repeat concussions suffered by professional football players. The settlement saves the league the negative publicity of a public trial and any admission of guilt. But the agreement could cost the organization upwards of $1 billion over the next six decades in payments for baseline testing, concussion research and education, and damages paid to ex-players with a related chronic condition, such as CTE or dementia, developed as a result of trauma suffered on the football field.
The NFL’s collaboration with GE, which began in 2013, is part of a four-year, $60 million research investment—$30 million of which comes from the NFL and $30 million from GE. That total includes $20 million designated to support the Head Health Challenge competitions and a $40 million R&D program aimed at evaluating and developing next-generation imaging technologies that would enable treatments to be targeted to patients with mild TBI. The latter is focused on a whole-brain approach, with the aim of determining the key MRI biomarkers for potential diagnosis, outcome prediction, and therapy management.
According to Alan Gilbert, director of Global Government and NGO Strategy at GE healthymagination, GE is developing a new MRI scanner that’s optimized for the management of TBI and is conducting a clinical study around TBI imaging biomarkers. But the company is also interested in the broader implications of this research in the field of neurological disease. “What we strongly believe,” says Gilbert, “is that what we learn in [the TBI] space is going to help us better understand what’s going on in patients with other neurological diseases, such as ALS, Parkinson’s, and Alzheimer’s. We believe these diseases have more in common than not,” he notes, “and we’re actually already seeing that this is the case.”
GE Seeks to Stimulate Premarket Creation and Exploration
The Head Health Challenge gives GE a chance to look at some early development work in this area that it otherwise would not have access to, says Gilbert, who stresses the open, no IP in/no IP out nature of the arrangement between GE, the NFL, and the contestants. All of the entrants were evaluated by an outside panel of experts, he notes, who measured the companies against their own criteria with respect to the questions they sought to answer, how they were pursuing those goals, and how far they had gotten. “We’ve seen in excess of 1,000 innovative ideas come through the program,” he says.
Although separately, GE’s venture arm looks at more than 600 ideas and makes about six or seven investments per year, GE healthymagination is really about “premarket creation and exploration, even before venture,” notes Gilbert. “It’s exciting to be able to look at all these early start-ups and academic groups because they are the ones developing the IP that will turn into those [venture-funded] start-up companies. That’s why we’re doing this.”
As for the differences between the three Head Health Challenges, Gilbert points out that Challenge II, which is focused on protection and preventing head injuries, deliberately sought out later-stage ideas that could be commercially available within a two-year period, while Challenge III was borne out of efforts around Challenge II and the need to develop new energy dissipating/dispersing materials. “So in Challenge II, you’re actually talking about a new helmet design, for example, but in Challenge III, it could be the materials that go into that design.”
Challenge I, however, was quite a bit different, with its focus on early diagnosis and intervention. Gilbert says GE was well aware that many of the technologies being considered in the Challenge I phase—such as biomarker blood tests, for example—would have to undergo FDA approval and thus would involve a “longer road to demonstrated commercialization.” However, some of the Challenge I finalists have “near-term potential” and could be in the ER, or possibly even on the sidelines, within a few years, he says.
BrainScope Brings EEG Brain Analysis to the Point-of-Care
One company that fits that criteria is BrainScope, which is combining a disposable electrode array with a powerful new analytics tool to provide a way of analyzing EEG (electroencephalogram) brain signals at the point-of-care. BrainScope already has FDA 510(k) clearance (granted in November 2014) for its first-generation device, the Ahead 100 (for use by physicians as an adjunct in diagnosing acute TBI in adults being considered for CT), and in May of this year, the company gained clearance for a next-generation version, the Ahead 200.
Development of both of those devices was supported in large part by the DOD, with an aim toward assessing soldiers and ex-soldiers with suspected TBI. But the company also is expanding its efforts in the area of sports-related concussion, with help from GE and the NFL.
According to BrainScope CEO, Michael Singer, the company’s technology was originally developed in the brain research labs at New York University School of Medicine by husband-and-wife team Dr. Leslie Prichep and Dr. E. Roy John, and “is a prime example of translational research.” (Prichep recently joined the company as chief scientific officer.)
BrainScope began operations in 2006 and Singer took over as CEO in 2008. But the company really got started on its current application in TBI in 2009. “When we first started,” notes Singer, “the concept was to use a handheld, rapidly applied EEG to assess any form of neurological abnormality. When I joined the company, we looked at the clinical data and it was quite evident that one of the most compelling areas where we were seeing very strong clinical correlation was with traumatic brain injury.”
 The technology itself consists of a standard EEG electrode array incorporated into a proprietary headset, which is placed on the forehead (see Figure 3). As the test is performed, classification algorithms interpret the EEG data signals to determine whether or not the patient has a TBI. The second-generation version of the device uses an off-the-shelf smart phone as the data processor and a disposable EEG headset. The EEG array plugs into the smart phone and the headset plugs into the EEG. Start-to-finish, it takes only about 10 minutes to run the test, Singer says, including about two minutes of prep time, and the results are immediately displayed on the smart phone screen.
The technology itself consists of a standard EEG electrode array incorporated into a proprietary headset, which is placed on the forehead (see Figure 3). As the test is performed, classification algorithms interpret the EEG data signals to determine whether or not the patient has a TBI. The second-generation version of the device uses an off-the-shelf smart phone as the data processor and a disposable EEG headset. The EEG array plugs into the smart phone and the headset plugs into the EEG. Start-to-finish, it takes only about 10 minutes to run the test, Singer says, including about two minutes of prep time, and the results are immediately displayed on the smart phone screen.
The algorithm is designed to identify very specific EEG signatures or features (electrical activity patterns in the brain) that show up after a blow to the head. The company has looked at over 5,000 patients in ERs across the country to validate the test and has been able to correlate specific EEG signatures with both clinical symptoms and structural patterns seen on CT. “It’s clear that there are not just one or two [distinctive EEG features], says Singer, “but there’s a fairly broad array of features that present themselves when there’s a brain injury.”
The initial aim of the current system is to help physicians determine which patients with suspected TBI should go on to receive a CT scan. The company uses a binary classifier in its first, cleared products, which classifies patients as either likely CT positive or CT negative. Those in the CT positive group would most likely be sent by the physician to get a CT scan, while those classified as CT negative would be seen by the physician as at lower risk for TBI and thus could safely avoid the radiation exposure and costs of a head CT.
The technology also has the potential to determine the severity of the brain injury, although Singer stresses that’s currently beyond its existing FDA indication. But, the binary classification system, he argues, “already falls into the pre-hospital arena. Because certainly if the clinician is assessing a patient to make a decision about whether or not to put them into an ambulance, then there’s no question this could be used right then and there.”
BrainScope has focused much of its efforts to date on military applications for its technology, a decision the firm made in 2009 because the “clinical data was so compelling” and because of the “enormity of the need,” emanating from the wars in Iraq and Afghanistan, says Singer. “All of that was paid for by the DOD as well as private funding,” he notes. “And we’re very proud of that significant public-private partnership—we think of ourselves as being a unique example there.”
But the firm also gradually expanded into the sports concussion arena, and to date, has amassed six years of sports studies, resulting in three peer-reviewed publications on the technology in sports (in addition to twelve peer-reviewed publications on the clinical utility of the technology in the acute assessment of TBI). “What the DOD and GE and the NFL are funding us to do,” explains Singer, “is take the technology and push it beyond the structural and functional [injury] to take a longitudinal view, looking at it not only from the time the patient has hit their head, right then and there, but the next day and the next week.”
From the sports studies the company has performed to date, Singer says it’s clear that there are signatures in the EEG that correlate with the persistence of concussion symptoms. And that’s why the NFL and GE and the DOD are so interested, he continues. “Because if you can remove the soldier or the athlete from the theatre or the game at that point in time, and get them healing without being exposed to more problems, then the better off you are.”
The com pany is currently undertaking three sets of clinical studies. It is continuing its acute-TBI studies in US ERs (work funded through private investment and DOD contracts), in order to improve its existing structural brain injury classifiers. It is also continuing to develop its concussion assessment system and is looking at the system longitudinally in adults (work also funded through private investment and by DOD contracts). And, it is looking at the technology in the adolescent athlete population (ages under 18) and plans to conduct studies in collaboration with US high schools (funded through private investment and awards from GE and the NFL). The firm will be assessing severity in its concussion studies as well as time to recovery, which are “two key elements,” Singer asserts .
In addition, the company is interested in expanding the technology to other neurological disorders, including stroke, seizure, and cognitive decline. When he was first evaluating the technology, Singer says stroke stood out as a very compelling opportunity—and came in a very close second to TBI. The company looked at its structural brain injury classifiers on a cohort of stroke patients, he says, and found that without altering the algorithms at all, the system was able to accurately detect the presence of stroke—whether hemorrhagic or ischemic. This could eventually lead to a rapid-assessment test for stroke, although Singer says that would require a “very significant investment.” The company also has a good deal of intellectual property around cognitive decline, Singer says, which is another area BrainScope “is extremely interested in.”
Although BrainScope has FDA clearance for its acute-TBI system, it has not yet launched products on the market, but is focused at present on gathering more data to improve system performance, further validate the technology, and broaden its reach. “The key for us,” notes Singer, “is getting data. The bigger and broader the database, the stronger we are. So this is both aggregating and validating data at the same time.”
However, one of the company’s key goals is to launch a TBI product on the US market in 2016. “We’re looking to use the Ahead 200 as the core of that product,” notes Singer, who says the technology will be applicable to a variety of markets, both domestic and international, as well as a variety of uses. “We expect it to be applicable not only in the ER, but also in the prehospital areas, like sports locker rooms and pre-ambulance, urgent care clinics, etc.” The military also will remain a fundamental market for the company, he says, “but our intention is to sell it both in the military and civilian markets.”
“We want someone to use the BrainScope technology as their first-line of assessment to determine if a person has suffered a TBI, and to give the clinician a significant amount of data that they can use to make an appropriate decision as to how they would handle their care.”
To date, BrainScope has received upwards of $30 million in government contracts and awards, and it has more than matched that amount in private funding, says Singer. “We have 92 issued and pending patents all around our technology,” he notes, “so we consider that to be a pretty good barrier to anyone that would want to get into this space.”
But, he continues, it’s a daunting challenge even without that IP barrier. “To be able to aggregate patients into the database—you’re talking about major clinical studies, and to have the technical knowledge to put those into classification algorithms and get it through the regulatory process—it’s quite a challenge. We’re proud of how far we’ve come. We’re in the early days and we’re seeing major breakthroughs.”
Banyan Biomarkers: Building a Pipeline of Blood-Based Neural-injury Markers
While BrainScope works to develop noninvasive EEG signals into a POC test for concussion and TBI, Banyan Biomarkers and Quanterix are both focused on detecting neurological markers in the blood.
Founded in 2002, with facilities in San Diego, CA, and Alachua, FL, Banyan Biomarkers is a spin-out from the University of Florida (UF) McKnight Brain Institute, where the company’s scientific founders, led by Dr. Ron Hayes, performed instrumental research in TBI (Hayes was head of the Institute’s Center for Traumatic Brain Injury). The goal of that work, says Jackson Streeter, MD, Banyan’s CEO, was to uncover brain-specific biomarkers that could be used to develop the first-ever POC diagnostic test for TBI.
Streeter joined Banyan five years ago. He had previously evaluated some work the firm did in the field of stroke, and recognized, he says, that the company’s technology was “potentially groundbreaking.” (Interestingly, Streeter’s background also includes a stint as a Navy flight surgeon and a commander with the TOPGUN Navy Fighter Weapons School.)
Researchers at UF performed the early TBI biomarker discovery and preclinical work, and once the company was spun out and the biomarkers were licensed, Banyan conducted human feasibility studies—supported by grants from the NIH and DOD—to determine if the markers the researchers had identified could be detected in humans, first in the CSF and then in the blood. Banyan performed feasibility studies involving several hundred patients, Streeter says, and was able to identify two proteins—Ubiquitin C-Terminal Hydrolase-L1 (UCH-L1) and Glial Fibrillary Acidic Protein (GFAP)—that cross the blood-brain barrier rapidly after injury and can be detected in the blood serum using ELISA (enzyme-linked immunosorbent assay) methodology. Banyan is partnering with established clinical laboratory companies on development of commercial TBI assays, and in August 2014 announced a partnership with Abbott Laboratories, which has licensed the two biomarkers and is developing the TBI assay to run on its iSTAT POC ELISA test platform.
In February, Banyan completed enrollment in ALERT-TBI, a 2,000-subject, multicenter, international study of head-injury patients with suspected TBI, funded in large part by a $26.3 million contract from the DOD. All patients in the study received a CT scan and a blood draw within 12 hours of injury. The blood samples will be screened for the two biomarkers and those results will be correlated with the CT scans, which will be read by three independent neuroradiologists. Streeter says the company will begin testing the blood samples as soon as the ELISA assay platform is finalized, which is anticipated before the end of this year.
The study outcomes are expected to be available in Q1 2016. The company will use that data as the basis for an FDA PMA application, seeking its first indication for the markers as a blood test in the ER to identify head-injury patients at high risk of TBI who need to get a CT scan. (The test requires a PMA because there is no predicate assay for this indication.) That first PMA will be submitted using an in-house ELISA test kit developed at Banyan; test platforms developed by partner companies will follow.
The clinical need for such a test is great, says Streeter, who notes that the brain is the only major organ in the body that can’t be analyzed objectively with a quantifiable blood test. As a result, CT is currently the workhorse diagnostic methodology for brain injuries, but it is far from the ideal diagnostic tool. For one thing, he points out, standard CT is not very sensitive at picking up mild injury—in fact, it often won’t see it at all. In addition, since CT is currently the only tool available for TBI assessment, it tends to be overused. Nearly everyone today who presents in the ER with suspected concussion/TBI gets a CT scan, he says, but that raises issues, because CT is expensive and it exposes patients to a significant amount of radiation. “So there are a lot of compelling reasons to better identify patients who really need to get scanned versus those who don’t.”
Moreover, the current standard rating system for concussion—called the Glasgow Coma Scale—was actually developed for coma patients, so it is a very crude instrument, says Streeter. In fact, you can have a fairly significant number of concussion symptoms and still have a normal Glasgow Coma Scale. “You can have a normal clinical rating and a CT scan that doesn’t show anything, and yet you’ve got a lot of severe post-head injury symptoms— things like headaches and difficulty sleeping and concentrating. There really needs to be a better way to identify this injury, and that’s something we’re trying to do,” he explains. Banyan envisions a potential market opportunity for an accurate POC test that exceeds 10 million tests per year in the ER alone, and many more outside the hospital setting (see Figure 4).
things like headaches and difficulty sleeping and concentrating. There really needs to be a better way to identify this injury, and that’s something we’re trying to do,” he explains. Banyan envisions a potential market opportunity for an accurate POC test that exceeds 10 million tests per year in the ER alone, and many more outside the hospital setting (see Figure 4).
While the company was pursuing the ER indication, it also began looking into sports-related uses for the biomarkers, working with the athletic department and doctors at UF on sports-related concussion. The recent NFL/GE award is allowing the firm to expand that work. It is currently conducting a study in collaboration with the University that is collecting a variety of data on a number of different types of student athletes, including the men’s football team, the men’s and women’s basketball teams, and the lacrosse and soccer teams, with plans to add the swimming team members as a non-contact sport control group. In that study, the company is collecting baseline scans using MRI diffusion-tensor imaging (which Streeter says is a better tool than standard MRI for imaging the brain for concussion), post-concussion MRIs, baseline biomarkers, and post-concussion biomarkers, as well as a battery of neurocognitive tests. Over the course of the 2015-16 athletic season, Banyan expects to obtain baseline readings on some 300 athletes participating in the study and to collect data on about 30 concussions.
The study will look at a battery of over 20 different biomarkers—including UCH-L1 and GFAP. “Some of them, like inflammatory markers, are not necessarily brain-specific,” notes Streeter, “but it will be interesting to see how all these different markers relate and if you can get improvement in sensitivity with perhaps a panel of biomarkers.”
The company is also about to start enrolling in a hospital study looking at its two markers serially, over time. Most of the work the firm has conducted to date has been in the very acute phase—within 12 hours of injury, Streeter says, but “in the mild to moderate population, we’d like to look at some more kinetic data.” Ultimately, the firm hopes to correlate serial data with outcomes in sports-related concussion to provide information on athlete recovery over time.
Like others working in this field, Banyan is also interested in additional applications for its biomarkers outside of TBI, including stroke or any other cause of neurotoxicity, such as a chemical agent, Streeter says. “The markers we have are neural-injury markers, so we think they will have a big application in stroke, and that’s actually the next indication where we want to do large clinical trials.” (In fact, the company already has some preliminary stroke data, he says.) Another potential future indication is for neuro monitoring in the ICU. “It’s difficult to move ICU patients when they need a CT or MRI scan—just moving them around the hospital has risks,” notes Streeter. “So it would be really nice to be able to just check their brain function with a blood test.”
Before the company expands outside of TBI, however, it intends to raise a significant round of funding. In addition to obtaining over $100 million in grants and contracts to date, Banyan has conducted a two-part Series A round, raising a total of $10 million, primarily from a group of high net-worth individuals. Following release of the pivotal TBI trial results next year, the company plans to look at the possibility of conducting a crossover round prior to an IPO, and then using those proceeds to pursue the stroke indication.
Banyan is also reaching out to a number of corporate partners interested in using its biomarkers on their assay platforms. For commercialization, the company does not intend to integrate the test into its own hardware; Streeter says it makes much more sense strategically to partner with large companies like Abbott that have existing platforms in hospitals. But he also stresses that Banyan intends to partner broadly. In terms of the Abbott partnership, which is focused on a POC test, he notes that “POC is certainly an area that we’ve focused on, but we’re not limited to that.” In fact, Streeter says the firm is already working with other central lab companies besides Abbott, although it has not yet made those names public. When it comes to partnering, he says, Banyan has “opted for the Microsoft model.”
Quanterix: Ultrasensitive Immunoassay Detects Blood-Based Biomarkers
Quanterix is also developing a blood-based test for TBI, employing a unique, highly sensitive immunoassay platform. Quanterix was founded in 2007 with technology originally developed at Tufts University by Dr. David Walt (who also founded gene-sequencing company Illumina). The company has developed an ultra-sensitive diagnostic platform it calls Simoa (Single Molecule Array) that is able to detect individual proteins in a blood sample at single-molecule concentration levels using standard ELISA diagnostic immunoassay reagents and techniques. The primary difference between Simoa and conventional immunoassays is its ability to trap single protein molecules (bound to magnetic beads) in femtoliter-sized wells. Using conventional fluorescence imaging, the company says the system can provide a digital readout of each individual bead, yielding an average sensitivity that is 1,000-times greater than conventional ELISA methods with coefficients of variation of less than 10%.
Exactly how it does that is a bit complicated, but worth delving into. The company’s system performs both sample prep, which is similar to standard ELISA techniques, and detection. To prepare the sample, paramagnetic bead particles coated with the target antibody are added to the blood sample and detection antibodies containing an enzyme capable of generating fluorescence are then introduced to the solution to form an immuno-complex consisting of the bead, the bound protein, and the detection antibody. The beads are then concentrated by magnetic separation and washed. At low analyte concentrations, each bead will contain either one bound protein or none.
An enzyme substrate is then added and the sample is loaded into an array that consists of 220,000 tiny micro-wells, each of which is only large enough to hold one bead. The arrays are located on a disc-like detector chip (made for the company by Sony, based on compact disc technology), and each disc has 24 slices, so 24 different samples can be run on one disc. When the sample is applied to the array, anywhere from 10,000 to 50,000 beads will find a home in one of the 220,000 wells, explains Quanterix CEO and Executive Chairman, Kevin Hrusovsky. After the sample has settled, an oil is placed over the top of the disc, which seals off the wells and enables each well to become its own independent reaction chamber. The system can then analyze the fluorescence in individual wells or look at the outcome across the entire sample plane.
The Quanterix technology is both digital and analog, according to Hrusovsky. It can glean a specific signal/noise ratio for one bead in one well, “but even if all of the beads have greater than eight proteins attached to them [which could happen if there were very high concentrations of analyte in the sample], our technology recognizes that in its algorithms and it then looks at the entire surface area and treats it as one well, like the old [ELISA] technology does.”
That ability to look at individual wells or the entire array means the system has a powerful dynamic range, he says. “If you had just one molecule, one protein, in a 1 ml sample, our technology would be able to identify it with exquisite precision, but if there were thousands and tens of thousands, or even levels that approximate what the old [ELISA] technologies could measure, we could handle that as well.” According to Hrusovsky, the engineering that’s gone into the system is “quite sophisticated,” considering how miniaturized the technology has to be in order to achieve single-molecule levels of sensitivity. And, the technology is unique in the field.
While many companies developing next-generation clinical diagnostics platforms are focused on highly sensitive DNA- or RNA-based tests, the Simoa assay is a highly sensitive next-generation platform focused primarily on the detection of proteins. Proteins got pushed to the back-burner when DNA testing came to the forefront, Hrusovsky says, but many people now believe that protein-based tests are the best way to capture the many epigenetic and environmental factors humans are subjected to. And the Quanterix technology platform, he notes, is applicable across nearly every category of medicine.
“We were able to create an instrument that’s as sensitive as DNA for proteins,” he asserts, “and now we’re applying it to just about every biomarker you can find.” Over the past year, Hrusovsky says there’s been “incredible market adoption of the technology across pharma, biotech, and many of the universities, although most of the fanfare and excitement has been in the area of neurological disease.”
The test takes advantage of a key discovery in the neurological arena: that biomarkers can leak from the cerebrospinal fluid (CSF) into the bloodstream. Previously, researchers believed that the blood-brain barrier prevented any such exchange. Thus, they relied on invasive tests, such as spinal taps, to gain access to substances in the CSF. But Hrusovsky says they now know that miniscule levels of neurological biomarkers move fairly uniformly and predictably across the blood-brain barrier. And, he says, the company’s highly sensitive Simoa technology is able to detect them in the blood.
“What we’ve established,” he says, “is the ability to see these neuro-biomarkers [in the blood], both when people are healthy and when they’re sick.” That capability makes the technology “much more disruptive” in neurology than some of the other clinical categories, he notes.
For concussion and TBI, the company is focusing on several specific brain biomarkers, including the well-established markers tau, amyloid beta, and GFAP, as well as some new markers such as neurofilament light (NFL). Studies have shown a direct correlation between the degree of concussive impact and the level of these markers in the blood, he explains. For example, with tau, the highest blood biomarker levels occur rapidly after the concussion event and persist for about an hour. Over time, tau levels decrease; however researchers have found that persistently elevated levels (over six days) are strongly correlated with more severe concussions. Additionally, recent research from the National Institutes of Health (NIH) suggests that soldiers who experience three or more TBIs have significantly elevated baseline tau levels compared with soldiers who have suffered less than three TBIs.
Ultimately, the company envisions a POC concussion test that includes a panel of biomarkers. “Our technology right now can deliver this level of exquisite sensitivity, with precision, for as many as 10 biomarkers simultaneously,” he says, so we expect this to be a panel that will likely require only a finger prick and can be performed on the sidelines. That’s really the vision of the second award that we’ve just won from GE and the NFL.”
Some of the biomarkers Quanterix is investigating for concussion also may prove useful for other neurological disorders, such as Parkinson’s and Alzheimer’s. For that reason, there are a number of pharma companies interested in this work, notes Hrusovsky. Some of these companies have developed drugs that have been on the shelf for many years, he continues, because clinical trials in this area are so unpredictable and risky when companies are dependent on subjective assessments, such as cognitive tests, to monitor outcomes. “Now that we’re getting these quantifiable markers, there’s been an avalanche of interest in trying to figure out ways to treat these ailments.”
Like many others working in concussion and TBI, Quanterix began by investigating military applications for the assay. In fact, the company’s accelerator arm (which does studies for outside researchers) has performed work for the DOD, and researchers from the DOD and the NIH have purchased a good number of the company’s test kits to perform their own studies, Hrusovsky says.
The company performed numerous studies investigating concussions that occur as a result of blasts and was able to show an “incredible correlation” between the presence of its test biomarkers in blood and severe blast-related concussions. Following that work, the firm began to look at mild TBI, in more of a sports setting, and also was able to show “exquisite correlations,” Hrusovsky asserts. The next step, he says, is to use these markers to not only detect concussion as soon as it occurs, but also to determine when it is safe for players to return to the field.
Over the next year or so, Quanterix will be working to broaden its concussion menu to encompass a wider range of biomarkers, including some that may spike more rapidly than others to enable a rapid-detection test. “This second award [from GE and the NFL] is really allowing us to expand the test menu and then to run additional trials on a broader menu of patients,” explains Hrusovsky.
But instead of taking on the entire development effort itself, the company is relying heavily on outside researchers, such as those at DOD, the NIH, and elsewhere, who are performing their own studies using the Simoa technology. “What we’re doing ourselves is probably 5% of what is being done by many others who already have our instrument,” he says. Some of those researchers are looking at how concussions lead to CTE and how that links to Alzheimer’s disease or Parkinson’s. “There are so many powerful studies, with much bigger sample sizes being done by these investigators.” The company readily embraces this “groundswell approach,” says Hrusovsky, rather than attempting to bring all these tests to market by itself.
Beyond neurology, the technology has the potential to improve test sensitivity for many other clinical applications, Hrusovsky says, such as companion diagnostics for cancer and cardiac troponin tests. And, the platform is not limited to protein analysis—Simoa can also be employed for DNA and microRNA testing. (In fact, Dr. Walt, the company’s founder, is investigating the technology as a genomics-based blood test for breast cancer, with the aim of one day eliminating the need for mammograms.)
“We can take traditional ELISA assays and traditional ELISA antibody pairs and apply them to our technology and get a 1,000-fold improvement in sensitivity,” Hrusovsky asserts. And those tests can be run with very small blood samples, thus reducing test invasiveness. The ability to obtain such a dramatic increase in sensitivity without having to create a whole new assay technology to achieve it, “is part of the real power of it,” he says.
The company currently has relationships with several commercial entities that are using the test platform for various applications. In late 2012, Quanterix signed a strategic partnership with French in vitro diagnostics (IVD) company bioMerieux, granting bioMerieux exclusive worldwide rights to the Simoa technology for clinical laboratory IVD testing and for industrial applications. At the time, bioMerieux took a $15 million initial equity stake in Quanterix, and the deal also provided Quanterix with milestone payments and sales royalties.
Quanterix also has agreements in place with several companies that are using the Simoa platform for laboratory developed tests (LDTs), including Rules-Based Medicine (RBM), a division of Myriad (which offers Simoa-based LDTs to the pharma/biotech research community in its CLIA-certified lab in Austin, TX), and Quintiles. “We’re very focused on allowing as much access to this technology as possible,” says Hrusovsky. The LDT tests span a variety of clinical applications, he says, including autoimmune diseases, cardiovascular, and oncology (Quanterix also collaborated with Beth Israel Deaconess Medical Center on a study published in August in the Journal of Clinical Microbiology that validated the technology for detection and quantification of C. difficile toxins in stool, suggesting possible uses in the infectious disease arena).
The company is still weighing its commercialization options for a concussion POC test, and whether it will partner with another firm to commercialize that test or market it itself. “We’re still early,” says Hrusovsky, “but there have been a lot of interested parties.”
Quanterix has received a total of about $50 million in funding to date, including the equity milestones from bioMerieux and three venture rounds (Series A through C), all of which have been up-rounds, Hrusovsky says. The next round of funding, a crossover round, will be later this year, which would set the company up for an IPO sometime in 2016, notes Hrusovsky. Sales revenues also have been ramping up—the firm brought in about $5 million in revenues in the first half of 2015, which Hrusovsky says is more than in all of 2014. He expects “a very significant ramp” between 2016 and 2021, with revenues reaching $150 million in that time frame. “We have a lot of IVD revenues that will be kicking in on some of those outer-bound years from our relationship with bioMerieux, but the RUO [research-use only] market is also going to be very robust for us over the next three to five years,” he says.
Hrusovsky joined Quanterix as executive chairman in June 2014 and was appointed CEO the following March. He previously served as president of PerkinElmer Life Sciences & Technology and CEO of Caliper Life Sciences (sold to PerkinElmer) and Zymark (sold to Caliper). Caliper provides laboratory instruments, reagents, tools, and drug-discovery assays (the company was a pioneer in microfluidic lab-on-a-chip technology) for pharma/biotech research use. Prior to that, Hrusovsky served as president of FMC Corp.’s Pharmaceuticals and International Agricultural Products, and he held management positions at E.I DuPont de Nemours, so his background and contacts draw heavily from the pharma arena, which has proven to be a plus for Quanterix. In fact, about 70% of the firm’s rapid growth in the past 12 months has come from pharma/biotech RUO, he notes.
“But as time goes on,” Hrusovsky says, “it’s really the academic and government investigators that are truly showcasing some of the best, most revealing data. Our technology really does impact, in v ery jaw-dropping ways, almost every therapeutic category. ”